Support, guidance & advice for todays primary carers
Smoke and Mirrors, but Mainly Smoke – The New Support at Home

Article by
Adjust text size:
It is slowly dawning on us all that there is a new Support at Home program that is being put in place to replace the old Home Care Packages (HCP) and the Commonwealth Home Support Program (CHSP).
This system needs to be installed into everyone by July 1st 2025. So, what do you want? The bad news or the not so bad news? To be fair there is some good news, but I will leave that until the end so we don’t all end up wanting to throw ourselves under a speeding bureaucrat.
So, the bad news and the not so bad news. It is said to be a simplification of the old system but it’s not. Downloading this new system into the software of my own brain will take months, even if I remain sane. Years, if a destructive virus corrupts my hard drive. It is called the “This is all too hard! Why is it so hard? Why are they doing this to me? I hate them all!” virus. But maybe this virus is inbuilt into the new system so we all give up. And maybe I have been watching too much Black Mirror. But honestly, changing an already complex system, into even more complex system while presenting it as simplification just gets my back up. I mean “back up” in the old-fashioned sense as in ARGGGHHH!!
Because sadly and inevitably, for the people who will have to implement the new program and the people who will need to use the new program, the whole new system is more complex and more difficult to manage.
We know this is a government exercise in cost cutting and making aged care more financially sustainable. But why does it have to be so punitive? And why, when it is so apparent to everyone who works in the sector that this new system will make access more difficult, waiting times for packages even longer, and delivering the services even costlier, is it presented as an improvement?
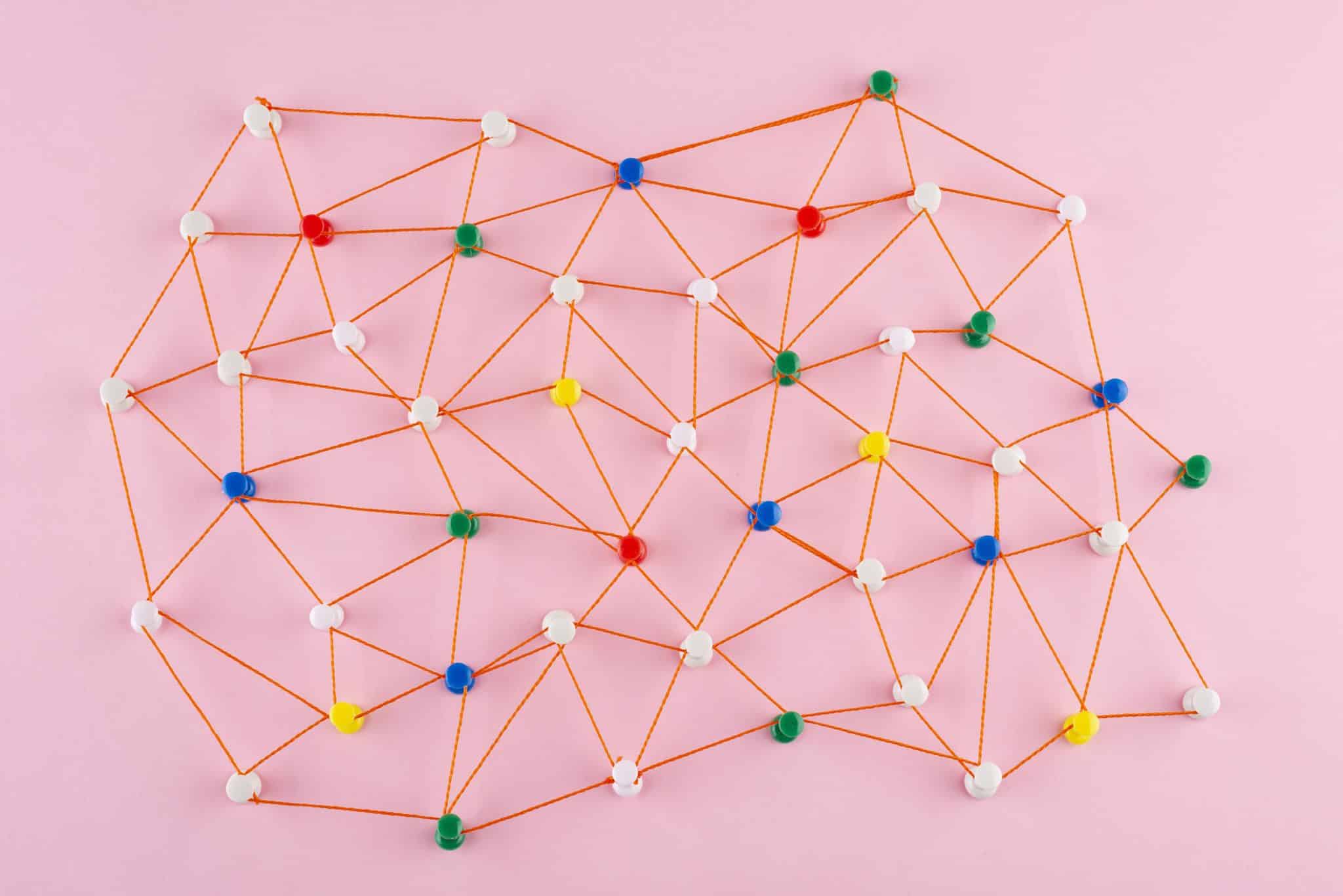
We won’t actually know the full impact of the new system before July 1st because much of the legislation is still in draft form. But one simplification they tout, is that the initial assessment, which used to be done by two different bodies (ACAT and RAS) is now “a single assessment for access to entry into aged care, and to access all government funded services. You only have to tell your story once”. So the story goes on the government website. One assessment, one story. This sound good!
But how on earth does this reconcile with the fact that instead of 4 levels of home care services there are now 8 levels? And, we have to be assessed or re-assessed for every level. That’s already 8 assessments rather than 4.
And within each level, services are divided into three different types:
- Clinical care (e.g. nursing care, occupational therapy, continence care).
- Independence (e.g. help with showering, getting dressed, taking medications, transport or respite care).
- Everyday living (e.g. cleaning, gardening, shopping or meal preparation).
When you are assessed, the assessor will determine with you what services you need. BUT, if on the day of the assessment you are assessed at a level 2 and the assessor ticks the box for ‘everyday living’ because that’s what you need at that time, and then the next day you hurt your wrist dandling grandchildren and you need help with a shower, you will have to be reassessed again, by an assessor, and the ‘independence’ box has to be ticked before you can access those services.
Apparently, this is based on the NDIS model, but with disability, needs are often stable and long term. Not in aged care. Needs can change from day to day, minute to minute. Suddenly you might have a wound, an injury, a sickness and you need acute care. You need different services immediately; you can’t wait for another assessment!
In the old system you would call your provider and say I need help showering, and they would swap out general support and organise some personal services for that afternoon. In the new system, the provider cannot do that.
In the old days you and your provider worked out your care plan. The provider can no longer do that. This is not a good change. Your provider needs to be able to respond to your needs and change your plan regularly.
So, let me just ask this question, if we have 8 separate assessments for the 8 different levels, and we also have re-assessments for the three different service types within each of the levels, how many assessments is that?
But wait, there are also 3 other levels of funds you can access. Sounds good!
These are:
- Assistive Technology and Home Modifications (AT- HM) – up to $15,000.
- A Restorative Care Pathway – up to $12,000.
- An End-of-Life Pathway – up to $25,000.
This extra funding is needed, but doesn’t that now mean there are 11 different funding levels? Each requiring a separate assessment. And each assessment then needs to be processed and approved, then a package allocated and implemented. How many months of waiting might that be?
Even with an unlimited supply of well-trained assessors, of which there is not. In fact, within agencies there is a turnover of assessors of about 70%. So, they use contractors. The assessment is complicated and to some degree discretionary, and the outcome of the assessment will be highly dependent on the skills of the person doing the assessment.
Which means our elders more than ever, need well-informed advocates to be with them during an assessment.
With regard to funding for an End-of-Life Pathway, I have always maintained that we needed a level 5 home care. We had four levels to support people to age in place, but no help for dying in place. You might have read my story about the last weeks of my parents’ lives. The grief and trauma of having to move them out of their home right at the end of their lives is still heartbreaking.
This new funding for End-of-Life care, palliative care, at home, is described as additional funding of up to $25,000 for your last 12 weeks (pushed to 16 if necessary – after that? The government is schtum). You need to be prognosed by a GP, followed by another assessment of course. It is described as ‘additional funding’ but it’s not. It is instead of the funding level you are already receiving. If you are on a level 8 which is $19,500 a quarter, then this is another $5,500 for 12 weeks, which is about $460 extra a week. If this is enough to help us die at home, which 90% of people want to do, we are yet to discover. The safe answer is “not”.
Nursing care is free but you need specialised palliative care nurses and practitioners for end-of-life, and providers are wondering where they are going to get them. Access to palliative care in Australia is already limited for so many, it is a postcode lottery as much as anything, so with all this extra demand how exactly is this going to work? Where will these wonderful nurses come from without a lot more funding for training?
There are many changes and some are complicated. For example, the assessment of your financial position needs to be understood. Your income and assets are now calculated much less generously with a view to you co-contributing much more generously.
This does not apply to those who have packages approved on or before September 12th 2024. Your package is grandfathered and there is a promise of ‘No worse off’.
Some changes feel merely tokenistic. For example, there are no longer ‘case managers’ they are now ‘care partners’. I mean really? Do we need this extra layer of gratuitousness? It will need more space than this column to explore all the complications of the new simplified Support at Home system.
However, we do need to know all the implications of the new rules. Having gone through all this with my parents in the old simpler system, my heart goes out to you all having to navigate this new there-be-dragons world.
But please give yourself lots of time, take it easy, how do you eat an elephant? And remember you are not alone.
The best place to get help is your provider, if you already have one. It is their obligation to support you through this transition. If your provider can’t answer your questions or help you understand the changes, then that is a massive red flag, and I would very seriously consider changing providers. They should be able to answer your questions by now.
If you don’t have a provider, or access to one, then I am sorry, but you may have to call My Aged Care on 1800 200 422. Or book a face-to-face appointment with an Aged Care Specialist Officer (ACSO) at select Services Australia centres on 1800 227 475.
TOP TIP
Have a book, your I.D, pour yourself a glass of wine, and call right on the knocker of 8am.
About Jean Kittson
Jean Kittson AM is an Australian performer, writer and comedian in theatre and print, on radio and television. Read more of Jean Kittson’s articles for Australian Carers Guide here.































The thing about all this that gets me is the continual assessments and not having my Care Manager or whatever they are now going to be called being in a position to react immediately to my needs or concerns. ACAT in New South Wales is literally a disgrace. You can never get them on the phone to make appointments. It’s a case of leaving message after message on an answering service until they finally get back to you, usually weeks later. Then they book an assessment months down the road and report to my Aged Care months after that. I am sure the New South Wales government is aware of this and also the Federal government and it is their way of ensuring funds are not spent by clients and they can then be clawed back as unused at the end of each quarter. A cynical attempt by the federal Government to address budget issues at our expense.
Having someone know your story and needs and lives in your community – someone to follow up phone calls, assessments, funding bodies and start date services, is what is needed. You would be surprised at conversations of dismissal from services because of wait times. Confusion is the overall outcome when dealing with so many levels and people. This then leads to overwhelm and stressed families. This frustration then is directed towards the elderly participant specially when the pressure is on when needed asap.. The carer or family member needs a degree in ‘aged care navigation’ to work through the system. Most the time families don’t know what they are entitled too even after the assessment and go without until a fall or emergency respite is needed.
You don’t know what you don’t know until you’re faced with it. Usually problems happen at weekends and late evening why not a phone service ,that we can use instead of ringing triple O. I am now in my 80, s and caring for a husband with a husband
With dementia and recently
Came upon “Care to Serve they arranged for almost immediate respite which gave us such relief and I did an information course which was invaluable to us. My husband had quality care ina nursing home for two weeks in Amur sing home .
Really appreciated reading your comment, as a Case Manager (pending Care Partner) grrrr my friend has gone through three assessments in order to get to his so call one stop shop assessment, he has a letter from an Orthopaedic Surgeon stating he has advanced arthritis in both hip causing great pain and discomfort. He stated my partner struggled to dress himself, struggles with transfers, unable to bend or do stairs. the last two assessors did not even look at the OH & S aspect of his home, which is a high risk and have allocate him a level 1. He can not bend, so he can not clean his home, do his garden, struggles walking, shopping, has no internet access or little connectivity, so how can they justify he only needs a level one. Does this mean if he gets a hip replacement down the track he will have to be assessed again in order to get personal care or other services he will need.
I was diagnosed with Herpes four years ago. For over two years, I relied on prescribed medications and treatments, but unfortunately, my condition continued to worsen. The flare-ups became more frequent, the discomfort increased, and even simple daily tasks became difficult to manage.Last year, out of desperation and hope, I decided to try a herbal treatment program from NaturePath Herbal Clinic. Honestly, I was skeptical at first, but within a few months of starting the program, I felt some changes. My discomfort eased, my energy levels improved, and I felt I had more control over my daily life again.It’s been a meaningful experience for me, and I feel more like myself than I have in years. This is simply my personal story. You can visit their website at http://www.naturepathherbalclinic.com
whatsapp +27604189106